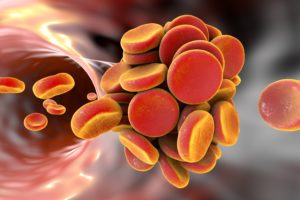
 Your heart pumps the blood through your arteries and then returns it to the heart where the process starts again. Blood is constantly flowing throughout the body. When motion and current cease blood can become stagnant, resulting in the possibility of blood clots.
Your heart pumps the blood through your arteries and then returns it to the heart where the process starts again. Blood is constantly flowing throughout the body. When motion and current cease blood can become stagnant, resulting in the possibility of blood clots.
When the body is injured in a way that cuts or punctures, in order to stop the bleeding a blood clot can sometimes form. Usually with no ill effects. There are times, however, when they form in locations they’re not needed in. Because of this early detection is important though recognition of symptoms and signs.
Learn the warning signs
Swelling
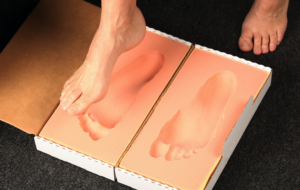
Developing a DVT (Deep Vein Thrombosis) also known as a blood clot in your arm or leg you could experience swelling. Risk factors for DVT include recent surgery, being stationary all of the time, or sitting on a plane at high elevation without movement for a long period of time.
Heart Palpitations
If you develop a clot in your lungs (a pulmonary embolism) it slows down your O2 rate. This causes your heart rate to speed up to make up the difference in the amount of O2 received.
Pain
Your entire body runs because of blood circulation. It requires it in order to move. A blood flow blocking clot can cause inflammation which leads to severe pain in the limb.
Color Changes
If you notice that an area in your body turns red or blueish, has a red streak, or becomes overly itchy, you may have a blood clot.
Breathing Problems
This can also be a sign of a lung based blood clot. You may have a deep cough or even cough up blood. Pain in the chest and dizziness Dizziness are also signs. Seek treatment immediately.
Elevated Blood Pressure
A kidney based clot can keep the kidneys from functioning properly and negatively influence the ability to process waste, removing it from your body. If left untreated it can cause kidney failure or higher than normal blood pressure.You may also notice you have a hard time breathing, leg swelling, blood in your urine or a fever.
Nausea or Vomiting
If a clot occurs in the veins that blocks the blood from your intestines, it can result in nausea, vomiting, blood in the stool, diarrhea, and stomach pain.
Never take a potential blood clot lightly. If you believe you may have a clot please call your doctor immediately or head to the nearest ER.
Problems Seeing and Speaking
A brain based blood clot can cause feelings of weakness, vision issues, speech problems, and even lead to a stroke.
If you are in the Tampa, Florida area and looking for a great Vein Specialist or Cardiologist please consider Tampa Cardiovascular Associates. Give us a call at (813) 975-2800 or visit online at www.tampacardio.com.

 It’s a fact that as we age our bodies do change. wrinkles and creases may begin to appear, skin loosens, our hair may grey. But what about varicose and spider veins? Many may consider it as well a badge of ageing, but the truth is that spider veins and varicose veins are not simply normal effects of time. They are the result of venous insufficiency. Vein Disease.
It’s a fact that as we age our bodies do change. wrinkles and creases may begin to appear, skin loosens, our hair may grey. But what about varicose and spider veins? Many may consider it as well a badge of ageing, but the truth is that spider veins and varicose veins are not simply normal effects of time. They are the result of venous insufficiency. Vein Disease.
 There are several different treatment options for spider veins. The one that stands out is sclerotherapy because it has stood the test of time and remains a top picked favorite of Vein Specialists as well as satisfied patients.
There are several different treatment options for spider veins. The one that stands out is sclerotherapy because it has stood the test of time and remains a top picked favorite of Vein Specialists as well as satisfied patients.
 Any of us who have experienced the death of a loved one who was very close to us know that the grief felt is very real and palpable. But can you really die from a broken heart?
Any of us who have experienced the death of a loved one who was very close to us know that the grief felt is very real and palpable. But can you really die from a broken heart? 
 Varicose veins are an issue that most people never talk about.
Varicose veins are an issue that most people never talk about.
 If you live in pain with venous insufficiency issues such as varicose veins you are likely willing to try just about anything to get relief.
If you live in pain with venous insufficiency issues such as varicose veins you are likely willing to try just about anything to get relief.


 A glass or two of wine or beer when out with friends or attending a party doesn’t really make you a “drinker”. Just a social drinker, like most of America. That likely doesn’t have too much of an effect on your veins. But what if it becomes more than occasional or you are a moderate to heavy drinker?
A glass or two of wine or beer when out with friends or attending a party doesn’t really make you a “drinker”. Just a social drinker, like most of America. That likely doesn’t have too much of an effect on your veins. But what if it becomes more than occasional or you are a moderate to heavy drinker?
 Are you experiencing symptoms?
Are you experiencing symptoms?
 Don’t resign yourself to a life of leg pain with unsightly varicose veins.
Don’t resign yourself to a life of leg pain with unsightly varicose veins.